
The Aetna Choice network is large and comprehensive. You’ll be billed for any amount that exceeds the reasonable charge. If he or she doesn’t, benefits will be paid at the lower, out-of-network level AND only up to what Aetna determines to be the reasonable charge for the service. If your doctor refers you to another provider (such as a specialist), be sure to ASK if the provider belongs to the network.
#Aetna urgent care copay free
While you are free to use any provider, you save money when you use in-network providers. In addition, you must file your own claims and call Aetna when your doctor recommends care that must be precertified. The plan pays a smaller share of your expenses.

When you need care, simply choose the appropriate doctor and make an appointment. You are not required to select a primary care physician (PCP) and no referrals are required for specialty care. Under the Aetna Choice POS II Plan, you may receive care from any licensed health care provider. This plan offers both in-network and out-of-network benefits however, the plan’s reimbursement is higher when you use an in-network provider. It provides the highest level of benefits.
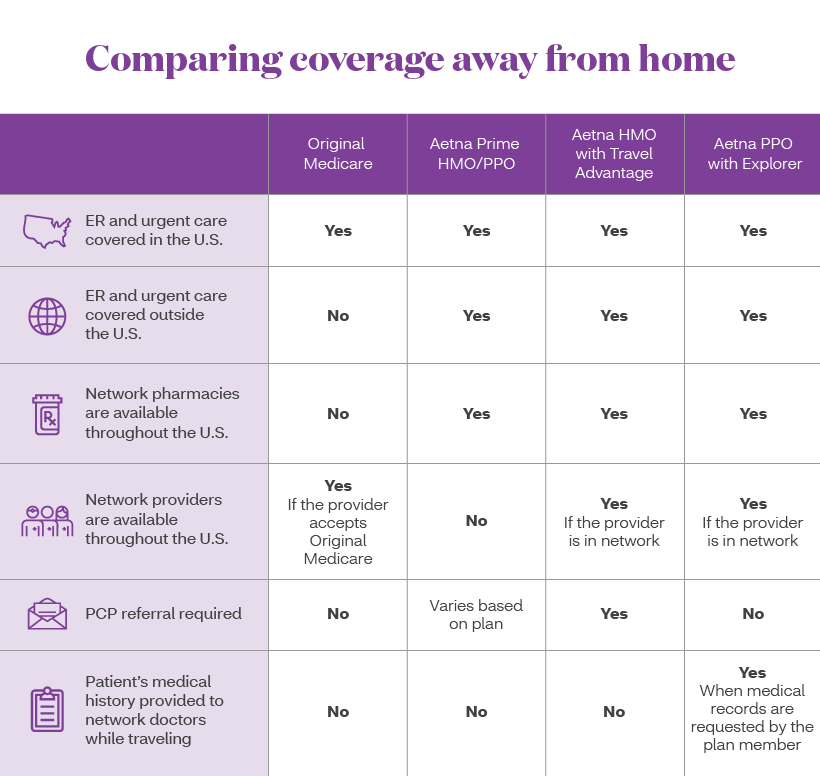
The Aetna Choice POS II Plan is a network plan that gives you the freedom to select any licensed provider when you need care.


 0 kommentar(er)
0 kommentar(er)
